FHIR HL7 Training on Binding Strength
Understanding FHIR HL7:
FHIR HL7 provides healthcare data professionals with a way to maintain organised, standardised information in an exchange format that facilitates seamless data management and sharing. A critical part of FHIR HL7 involves identifying official codes that facilitate seamless exchange.
Imagine trying to validate a medical record number within the FHIR HL7 standard. Your system must define it correctly by pulling data from source systems, such as hospital mRNA identification numbers or patient records. FHIR HL7 provides a structured approach.
Welcome! Today, we will explore FHIR, an HL7 standard used for healthcare data exchange. Since its initial creation over 40 years ago, multiple versions have been implemented in response to changing industry needs.
Beginning with HL7 Version 2, releases ranged from 2.0 to 2.9. Due to legacy systems, many systems still rely on older versions; FHIR HL7 presents an alternative method of interoperability.
FHIR (HL7) has undergone six major releases to date. Starting as Draft Standard Trial User-1 (DSTU1) for trial use, subsequent draft standards included Draft Standard Trial User-2 and three other releases, until STU3 became the final standard. Eventually, it evolved into Release 4, with R4B being available as a minor bug fix version; R5 was recently unveiled as its most up-to-date iteration.

Binding Strength in FHIR HL7
Let’s discuss FHIR and HL7, and their concept of binding strength. When working with FHIR HL7, value sets that define data structures will frequently arise; binding strength serves as the gauge by which to assess how closely systems must adhere to those predetermined sets.
FHIR HL7 utilises attributes such as code or codable concept when defining resources, unlike more conventional programming languages like Java or .NET, which include their own data types – a unique feature within healthcare interoperability.
Consider FHIR HL7 administrative gender, for example, HL7.org specifies codes such as ‘M’ for male, ‘F’ for female, and ‘U’ to indicate unknown. FHIR HL7 defines attributes with binding strength rules to maintain data exchange standards and consistency across data exchange channels.
FHIR HL7 Code System Resource
FHIR HL7’s value set resource is linked with its code system resource. This code system defines all possible values and plays an essential role in effectively structuring data.
Navigating a code system resource, for instance, you will encounter a URL representing that system, serving as its key identifier, allowing users to access specific administrative categories, such as gender.
FHIR HL7 requires each code system to have its distinct URL for easy reference when accessing resources. This ensures consistent value access when making reference queries.
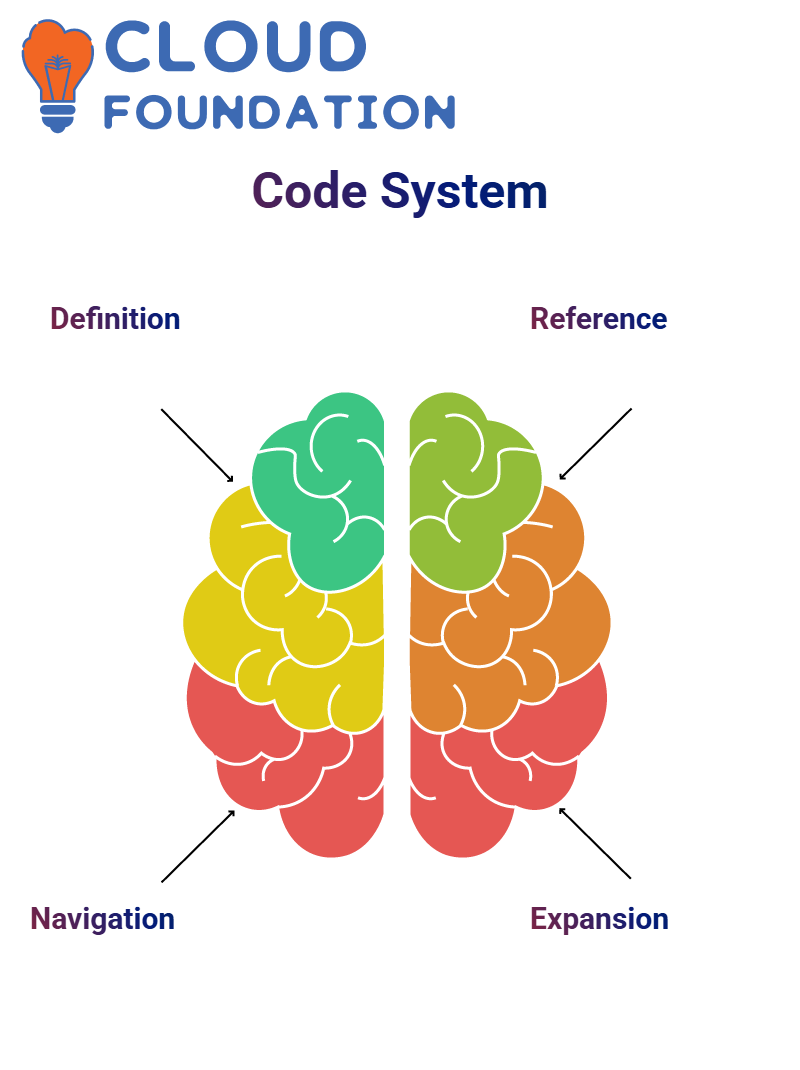
Creating and Extending Resources in FHIR HL7
FHIR HL7 allows users to create new resources by building upon existing ones. When adding codes for marital status categories, such as increasing their size by expanding them by adding new codes, these must adhere to predetermined binding strengths.
Extensible value sets enable users to copy existing structures, modify details, and introduce new codes flexibly, allowing the FHIR/HL7 ecosystem to accommodate evolving healthcare requirements effectively.
JSON-Based Patient Resources in FHIR HL7
Understanding how to structure an FHIR HL7 resource using JSON is vitally essential, since every resource follows an organised structure starting with its resource type designation.
When creating patient resources, it is essential to adhere to the JSON formatting rules. Attributes should be structured methodically while meeting specification guidelines to produce a clear and easily understandable representation.
FHIR HL7 resources rely on correct data types and formatting rules; primitive attributes, such as Boolean values, may follow a straightforward path, while complex attributes necessitate additional nesting within structured objects.
FHIR HL7 Identifiers
FHIR HL7 relies heavily on unique identifiers to ensure data uniqueness and integrity, enabling healthcare systems to differentiate patients, track data accurately, and maintain systems within an established structure. A well-structured identifier enables healthcare systems to identify patients more easily while maintaining integrity within a standardised framework.
FHIR HL7 Data Implementations
Data integrity should always be the top priority when implementing FHIR HL7 systems. Therefore, system validations must be conducted to confirm that medical record numbers correspond with predefined structures within this protocol and prevent inconsistencies from developing.
Mastering FHIR HL7 requires comprehending type structures, validating system codes, and ensuring seamless integration into healthcare applications. Adherence to best practices ensures reliable data management practices.
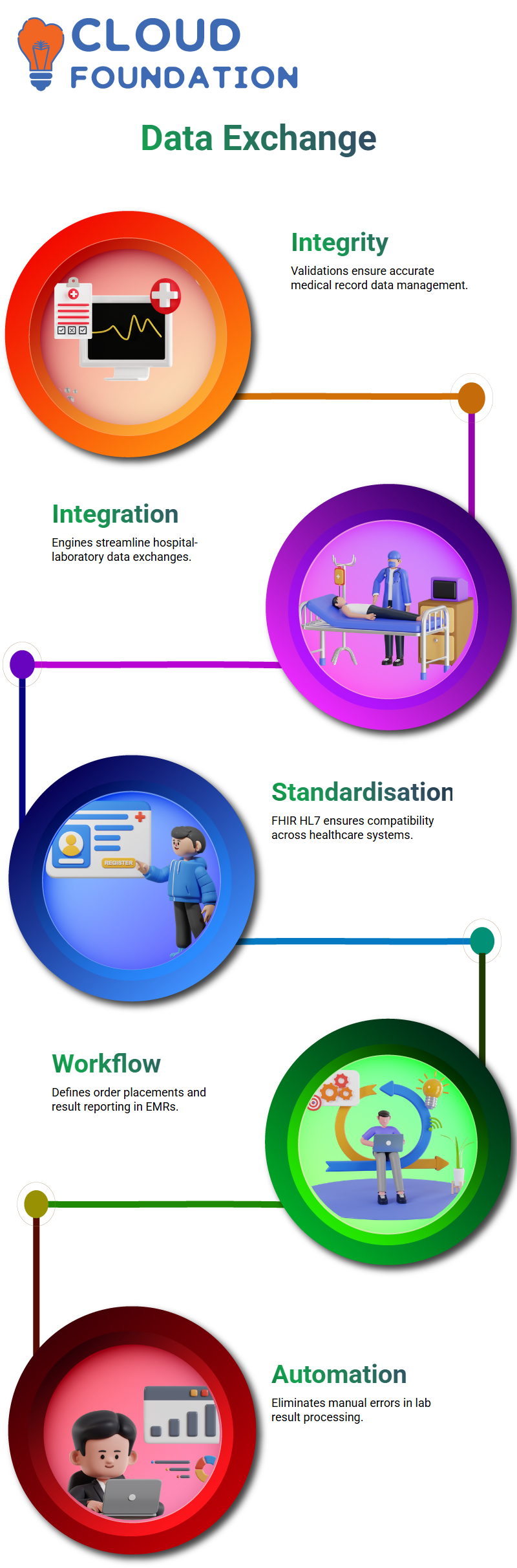
FHIR HL7 Integration Engines
Integration engines play a pivotal role in facilitating efficient data exchange between hospital systems and laboratories when working with FHIR and HL7.
My personal experience has taught me to successfully set up results and order integrations despite various hurdles along the way.
Hospitals typically initiate the process with an initial kick-off call to define requirements. During this call, the requirements and specifications for order placements in the Electronic Medical Record (EMR) are described, and these orders are then sent to laboratories for testing.
The results are subsequently sent back into the hospital information systems for reporting. Understanding exactly which lab products must be sent back is also key to effective workflow management.
FHIR HL7 helps facilitate these exchanges by standardising messaging formats, which enables healthcare providers to share patient data efficiently without compatibility concerns.
Standardising laboratory procedures ensures hospital systems can process laboratory results seamlessly without human interference or manual processing delays.
Customising Data Fields in FHIR HL7
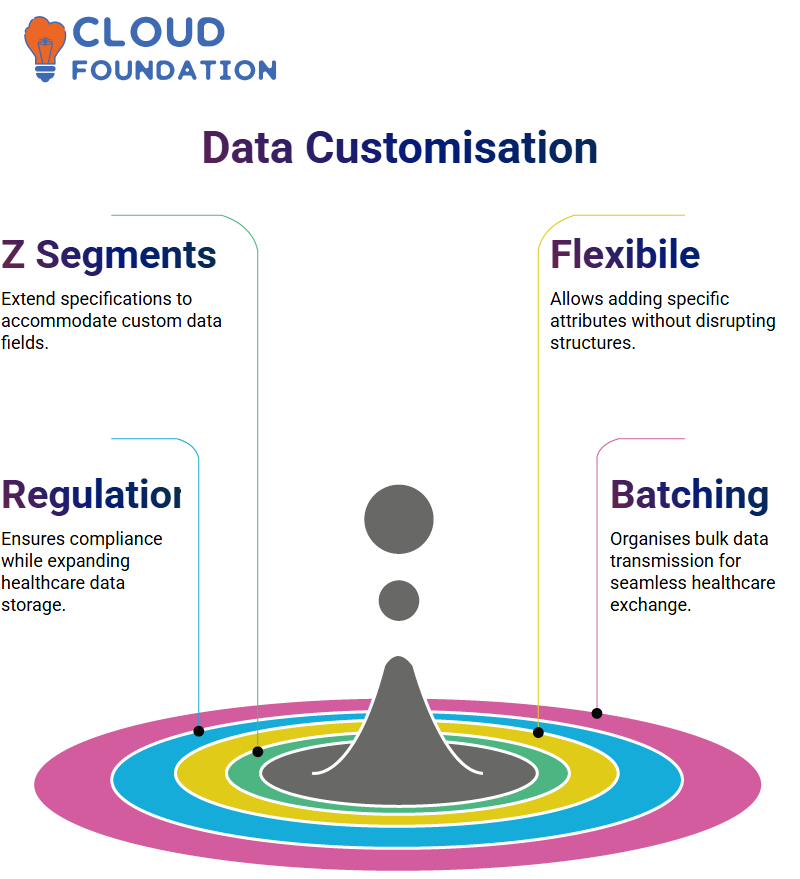
Z segments offer the necessary customisation solutions in this regard.
Suppose a placeholder for a specific data field doesn’t exist. In that case, we can use Z segments to extend its standard specification and add vital details, such as legal gender and preferred gender, without disrupting existing HL7 structures. This gives us more flexibility when accommodating specifics, such as legal gender or preferred gender considerations.
For instance, if a hospital requires additional components in its PID segment, it can define new fields at the end of its specification document.
FHIR HL7’s goal is to maintain the orderly storage of patient data while meeting regulatory standards, whether that means expanding fields or adding custom segments. FHIR HL7 offers tailored healthcare solutions explicitly tailored for every need in healthcare today.
Bulk Data Transmission in FHIR HL7
Hospitals occasionally need to send bulk messages using FHIR HL7’s structured batch process, necessitating an organised batch process in FHIR.
When transmitting multiple patient records at once, messages must be organised into batches to facilitate retrieval and organisation. Batch header and trailer segments play a vital role in maintaining data integrity during transmission.
FHIR HL7 specifications provide healthcare institutions with guidance on structuring bulk messages to streamline operations and efficiently manage patient orders, laboratory results, or imaging data. Structured batching within FHIR HL7 ensures smooth data exchange among systems interlinked by it.
Why is FHIR HL7 Faster and More Efficient?
FHIR HL7 was developed with speed and simplicity in mind. Traditional HL7V2 structures often necessitate dealing with multiple message segments simultaneously, making the process cumbersome. FHIR HL7, however, provides resources explicitly tailored to various functions, facilitating faster processing times and overall work efficiency.
FHIR HL7 provides systems with direct access to patient resources, eliminating unnecessary data exchange and streamlining operations. With such benefits in mind, FHIR HL7 remains the go-to choice for healthcare interoperability.
How Binding Strength Works in FHIR HL7?
FHIR HL7 defines four levels of binding strength for value sets: Required, Extensible, Preferred and Example.
Each level determines how strictly systems must adhere to predefined codes in that value set; for instance, if FHIR HL7 indicates this set has Required binding strength requirements, then systems are only allowed to utilise those defined codes within that value set.
Gender in FHIR HL7 requires adhering to specific values to guarantee compatibility across platforms.
FHIR HL7’s extendible nature offers users slight flexibility: users may add new values while maintaining predefined ones; for instance, marital status codes in FHIR HL7 can be expanded while still adhering to standard definitions.
FHIR HL7’s “Preferred” binding strength indicates systems should use the suggested codes when possible, but may reference another value set when necessary. On the other hand, “Example” binding strengths provide sample codes that users may modify freely as desired.
Value Sets in FHIR HL7
FHIR HL7 allows its users to extend value sets as necessary. For instance, if an institution needs to record additional information, such as specifying a person who is five times married, they can easily add an extra row to an existing value set.
FHIR HL7 ensures interoperability by assigning a defined URL to every value set, which leads back to its source, making modifications tailored specifically for user needs much simpler and enabling interoperability across systems.
FHIR HL7 remains an integral element of healthcare data standardisation. Acquiring knowledge of FHIR HL7 binding strength equips developers with all the skills needed to maintain structured data in real-world applications.
FHIR HL7 provides an effective structure for organising healthcare data. One key aspect is understanding value set resources, which specify allowable codes in specific fields within any system.
As you investigate a value set resource, you may encounter an initial URL that serves as its guidepost. At first, this URL might seem to lack associated codes, but don’t worry, you’ll soon realise its true worth!

FHIR HL7: Optimising Transaction Processing
The real-world implementation of FHIR/HL7 originated from a hospital information system that required processing 640 messages per second. In this context, batching was utilised as an optimisation approach instead of sending individual transactions.
By leveraging FHIR HL7 batching techniques, transactions can be combined, thereby reducing unnecessary authentication requests and enhancing performance. This approach demonstrates how FHIR HL7 facilitates the efficient streamlining of large-scale operations.
Healthcare data in FHIR HL7
In healthcare data processing, transmission, and storage play a crucial role in ensuring efficiency and accuracy. FHIR, an extension of HL7, provides a standardised framework that facilitates interoperability within healthcare systems.
FHIR, an extension of HL7, provides seamless communication among healthcare applications by harnessing self-contained resources.
In contrast to its predecessor, HL7V2, which requires multiple message segments to be structured separately for transmission, FHIR HL7 simplifies this process by prioritising only the data that matters most for transmission.
FHIR HL7 continues to develop with each release, such as R4 and R5, adding resources. Thanks to its adaptability, FHIR HL7 ensures seamless integration across various healthcare applications, making it a valuable asset in data exchange.
The increasing adoption of FHIR by healthcare institutions and developers underscores its significance. From optimising workflows to streamlining data transfers, FHIR HL7 provides a gateway for improved healthcare communication.
Healthcare Data Exchange in FHIR HL7
As healthcare applications demand API interaction, understanding FHIR HL7 becomes essential.
Status codes often play a crucial role in healthcare technology integration and data exchange; for instance, 200 indicates success, while 400 represents invalid requests. API documentation ensures seamless integration and data transfer from APIs within healthcare technology environments.
FHIR HL7 plays an invaluable role in transmitting patient data. If you need to add new patient records, sending data via the POST method is part of this process.
Healthcare applications must adhere to specific guidelines to facilitate the seamless transfer of data among systems, or interoperability issues may arise. Without standardisation in place, these challenges could arise.
Localisation in FHIR HL7 is also key. Recently, we encountered an implementation scenario in North America where regulations required hospitals to submit both preferred gender and legal gender data in an application requesting it. Successfully mapping such specific data within an HL7 framework ensures compliance and efficient communication between services.
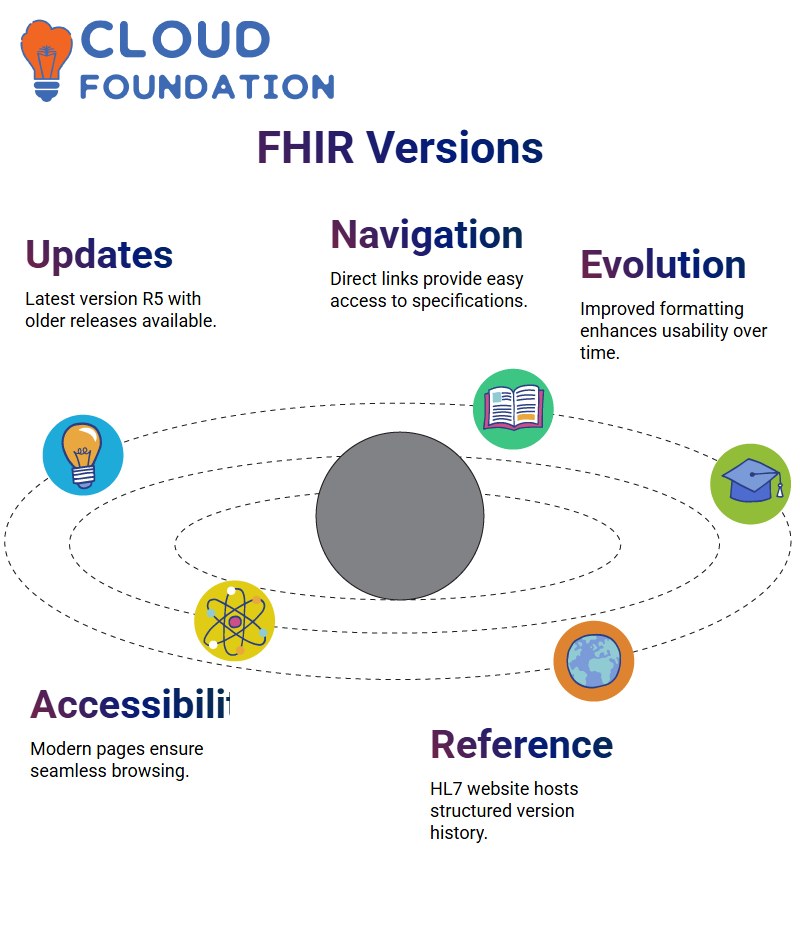
Navigating FHIR HL7 Versions
If you are researching FHIR HL7 specifications, the official HL7 website always hosts the latest versions available, typically R5. However, older versions, such as R4B, R4, STU3, and DSTU2, may also be found there.
Each version of FHIR HL7 features structured navigation elements. The home page provides direct links to these releases, enabling users to access previous versions easily.
Over time, FHIR HL7 pages have evolved dramatically. Their earlier versions featured basic formatting; now, however, they provide visual enhancement and user-friendliness, providing seamless access to specifications.
Real-World Deployments in FHIR HL7
Once testing has concluded, hospitals sign user acceptance agreements to officially implement FHIR HL7 integration into production mode, allowing them to receive actual patient records through the system and providing hospitals with efficient ways to process live medical data.
FHIR HL7 ensures structured data exchange in production environments, so laboratory results align seamlessly with hospital data models without discrepancies between data models and laboratory reports. Patients no longer require manual interventions for order tracking as the integration engine provides real-time messaging updates for order status changes.
FHIR HL7 plays an indispensable role in providing seamless hospital-laboratory integrations and minimising disruptions in medical data workflows. Healthcare providers can focus on delivering quality care rather than struggling to identify data inconsistencies.

Navya Chandrika
Author