FHIR HL7 Data Types Workshop Training
Understanding FHIR HL7 Data Types
FHIR HL7 data types are critical. An existing lookup table determines a third component; any deviation could cause a mismatch, resulting in the end application interpreting your information differently.
Under strict validation scenarios, such as Rhapsody’s software system, errors will be flagged according to the EDA schema.
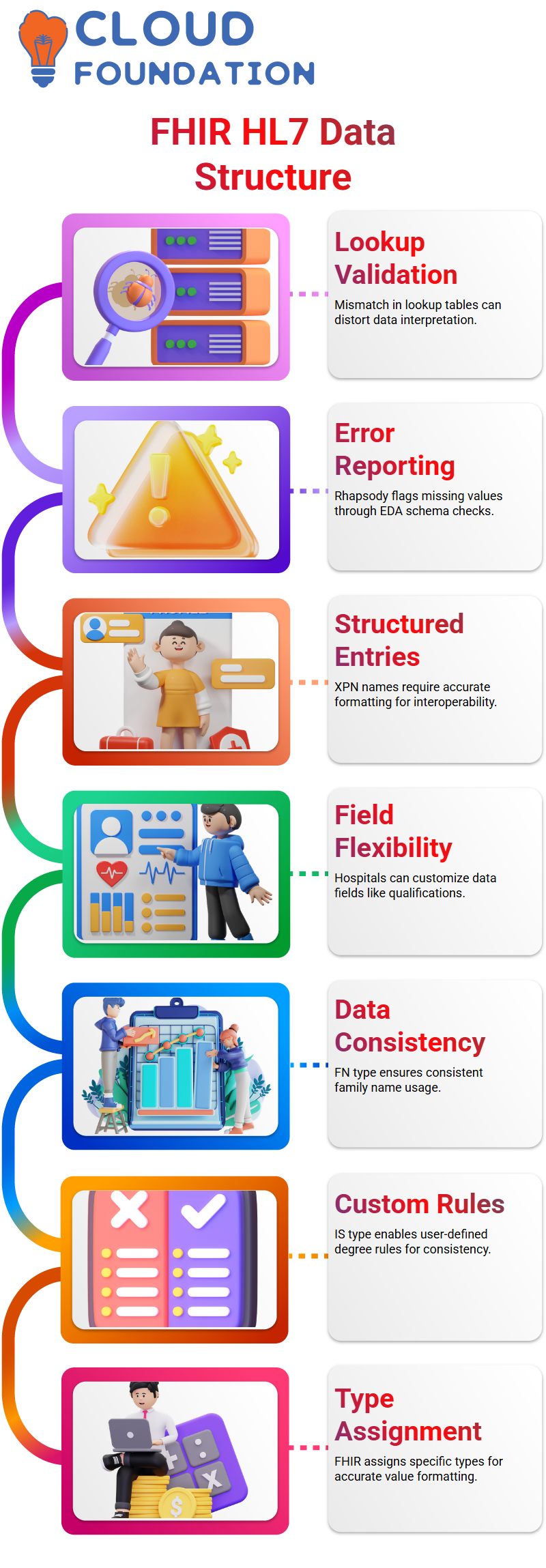
If Rhapsody cannot locate an expected value, an error report will be generated, ensuring compliance with HL7 specifications.
Defining FHIR HL7 Data Types
FHIR HL7 data types play a crucial role in structuring healthcare data. Hospitals have the flexibility to personalise specific fields, like degree qualifications, making data entry quicker and more adaptable.
FHIR HL7 assigns specific data types for values; family names use the FN data type to ensure uniformity across applications.
Some data types, such as extended patient names (XPN), require structured entries to maintain interoperability, making their correct definition crucial for accurate data exchange.
FHIR HL7 stands out in particular due to its support for user-defined data types, with IS being an example.
Hospitals can create their own rules using this IS data type by listing acceptable degrees, providing consistency while still permitting enough flexibility.
Primitive Data in FHIR HL7
FHIR HL7 divides data types into primitive and complex structures. Primitive types, such as strings, don’t contain subcomponents.
For example, when recording names directly inputted, such as ‘Mickey’, this would suffice as input data.
Complex data types often consist of several interdependent parts. To reveal whether an expansion exists, clicking its definition reveals any hidden layers – this structured approach ensures proper usage within FHIR HL7 applications.
Conditional Data Fields in FHIR HL7
FHIR HL7 introduces conditional fields, meaning their presence depends upon other components being present – for instance, assigning authorities must accompany universal IDs.
FHIR HL7 provides consistency across healthcare systems by structuring data for patient records in an easy-to-interpret format, making patient information readily available on healthcare systems.
Optional Fields in FHIR HL7
FHIR HL7 allows for optional fields, so if a hospital lacks information for one component, they can exclude it; however, keeping empty pipes to maintain data integrity remains essential.
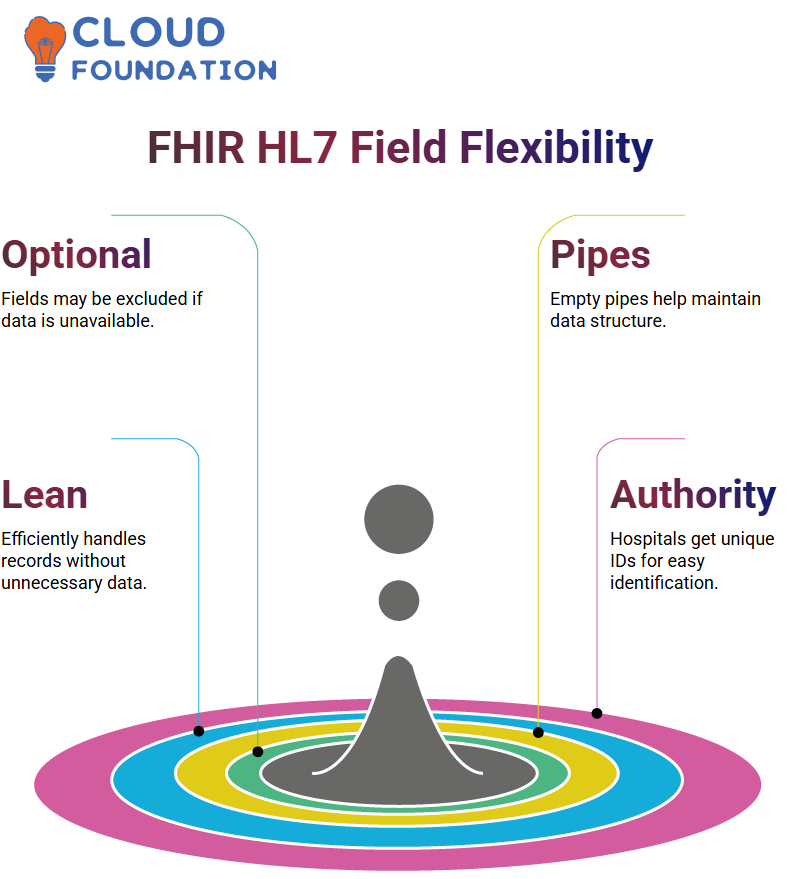
FHIR HL7’s adaptability enables healthcare applications to process data efficiently without extraneous elements clogging their records.
Authority in FHIR HL7
FHIR HL7 provides hospitals with a unique identifier to establish hierarchical identifiers within its framework, making hospital identification within this system much simpler and accurate. Hospitals use namespace IDs as unique identifiers.
Namespace IDs are essential when creating patient identifiers that enable hospitals to track records residing under FHIR/HL7. Without them, tracking can become nearly impossible, and records become more easily duplicated and less identifiable.
Component Separators and Their Role in FHIR HL7
FHIR HL7 uses special characters, such as parentheses (), to separate components within fields and distinguish different elements, such as an ID check digit string, which typically comprises four characters.

FHIR HL7’s flexible approach ensures that hospitals can easily incorporate different data types, such as English, Hindi, or other special characters, for multilingual healthcare systems.
FHIR HL7 Tables and Data Structure
FHIR HL7 utilises tables to organise information systematically. These tables define permissible values for various fields to prevent inconsistencies between values in these fields and those described in relevant HL7-specific books.
This helps ensure that valid values align with current industry standards and that all references are appropriately matched with any changes that may occur over time.
Legal names might be marked ‘L’ to create uniformity. FHIR HL7’s predefined structures enable faster data processing while reducing ambiguities within healthcare records.
FHIR HL7 and User-Defined Data Types
Name type codes are another crucial aspect of an HL7 structure; their seventh component relies on ID data types defined within a table for ease of implementation across implementation sites.
FHIR HL7 ensures that values originate from appropriate references, thereby promoting greater standardisation across implementations.
Backwards Compatibility in FHIR HL7
FHIR HL7 prioritises backwards compatibility to ensure that older implementations remain functional.
Versions such as HL7 2.1 may contain fields not widely utilised by modern standards, despite their continued presence within later standards, such as 2.9.
Hospitals operating on older infrastructure can utilise legacy fields with confidence, knowing that data migration will occur without disruption or interruption, thanks to FHIR HL7’s compatibility across versions and the integration of advancements.
FHIR HL7 Date-Time Format
FHIR HL7 provides an orderly process for recording dates and timestamps in patient records using 24-hour notation to eliminate confusion and ensure seamless interoperability.
This system ensures precise timestamps that eliminate ambiguity for smooth patient management.
Birth dates follow a DTM data type because this primitive type does not require further breakdown.
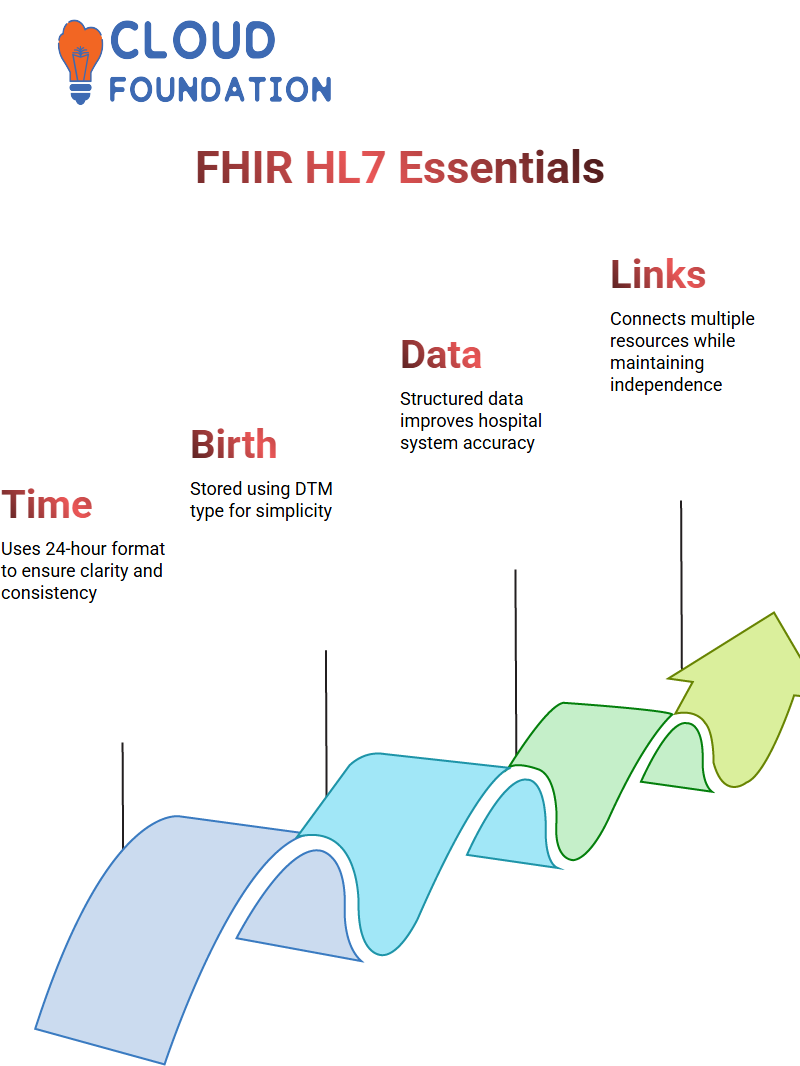
Hospitals that utilise FHIR HL7 benefit from structured formats that ensure accurate data capture.
FHIR HL7 Resource
As part of working with FHIR HL7, understanding how patient resources connect to other entities is of vital importance.
Here we explore the referencing concept, which allows us to connect multiple resources while still respecting their autonomy.
FHIR HL7 provides resources that are both self-contained and interlinked by specifications.
For example, ServiceRequest resources feature an attribute called Subject that references patients, groups, locations, or devices, thus maintaining consistency while increasing interoperability across healthcare data sets.
XML, JSON, and Turtle in FHIR HL7
FHIR HL7 provides support for multiple data formats, including XML, JSON and Turtle.
While the first two have become standard practice over time, Turtle remains less frequently employed.
FHIR HL7 provides structured examples to help beginners learn FHIR and HL7 quickly and effectively.
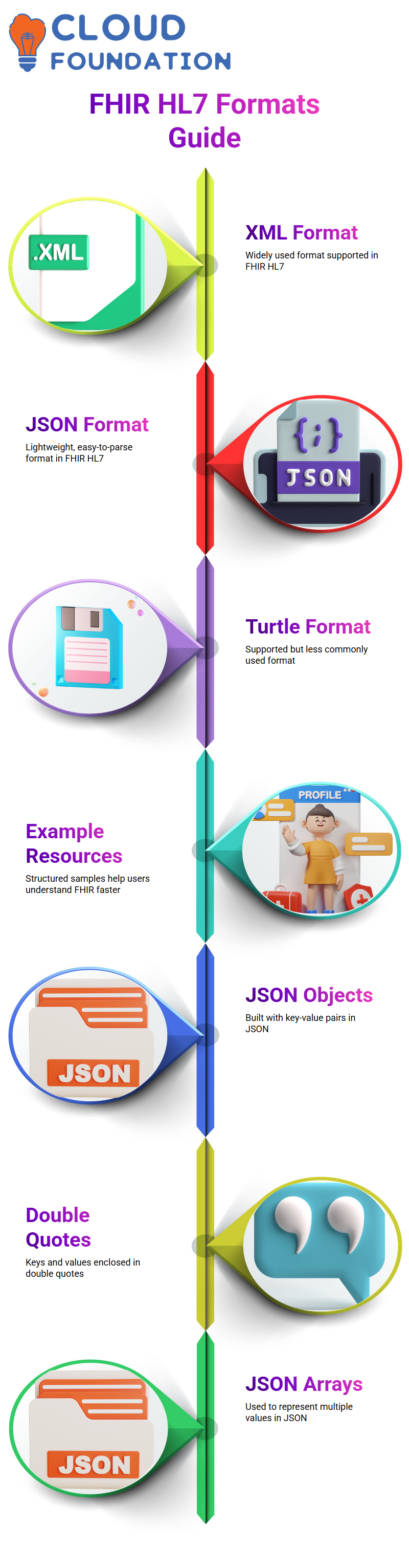
These illustrations showcase various formats of resources available, allowing practitioners to select one that best meets their needs.
JSON Formatting in FHIR HL7
JSON is an ideal format for FHIR and HL7 resources due to its lightweight nature and ease of parsing; therefore, understanding its structure is essential for crafting well-formed resources.
JSON objects consist of key-value pairs, with double quotes enclosing keys and values, as data types vary based on their types.
JSON arrays enable the representation of multiple values simultaneously, facilitating easier integration within FHIR HL7.
Breaking Down JSON for FHIR HL7 Resources
As soon as you start working with FHIR HL7 specifications, understanding JSON becomes essential.
It involves creating arrays, objects and complex data formats, which might initially seem complicated. However, don’t be intimidated; I’ll help guide you through it step by step!
FHIR HL7 operates under specific guidelines, meaning that resource definitions must adhere to these guidelines in terms of how resources are specified.
As we delve further into writing specifications together, I will ensure that each aspect of writing specifications is understood, making your learning journey smooth and hassle-free.
Object Arrays in JSONFHIR HL7
FHIR HL7 resources may contain arrays of objects. For instance, patient telecom attributes may have multiple entries regarding contact numbers that categorise them by personal and office.
JSON provides clarity and facilitates interpretation in FHIR and HL7 applications.

Vinitha Indhukuri
Author